 产业资讯
产业资讯
 药明康德
药明康德  2025-10-11
2025-10-11
 410
410
编者按:精神分裂症是一种常见且复杂的严重精神疾病,根据世界卫生组织的统计,全球约有2400万人受到影响。患者常常面临幻觉、妄想、思维障碍和社交退缩等症状,不仅剥夺了他们的正常生活,也给家庭和社会带来沉重负担。现有治疗手段虽能在一定程度上缓解症状,但仍存在疗效有限、耐药性和副作用显著等难题。近年来,精神疾病新药研发迎来突破,不仅为精神分裂症患者带来了数十年来首款新机制疗法,也开辟了精神疾病治疗的新方向。长期以来,药明康德始终支持精神疾病药物的研发,依托“一体化、端到端”的CRDMO模式,助力合作伙伴将科学突破高效转化为创新药物。在这个世界精神卫生日(World Mental Health Day),本文将通过一名患者的故事,走近这一领域的探索与希望。
点亮大脑中的“灯泡”
蒂姆(Tim)是一位20多岁的年轻人,自青少年时期便被确诊为精神分裂症。多年来,他接受过多种抗精神病药物治疗,但效果始终有限。药物还带来多种副作用:体重增加、过度嗜睡以及难以忍受的静坐不能(akathisia)。这让他逐渐失去了坚持服药的意愿。随着用药依从性下降,他的症状越来越难以控制。家人形容他越来越沉默寡言,陷入自己的世界,眼神空洞,又经常出现情绪激动并难以控制行为。蒂姆的生活似乎陷入了反复住院和生活状态紊乱的循环之中。
直到2024年,蒂姆开始使用Cobenfy(xanomeline/trospium)。他的变化几乎是立竿见影,短短数周,家人发现他眼中的空洞感消失了,取而代之的是久违的神采。医生将这种转变形容为“灯泡效应”(the light bulb effect):就像一盏久未点亮的灯突然被点亮,蒂姆的个性与活力被重新照亮,他的家人也第一次看到了希望。而这款给蒂姆和他的家人带来希望的新药也曾走过漫长而曲折的开发路程。

图片来源:123RF
原本用于治疗阿尔茨海默病,却发现意外疗效
让我们回到上世纪90年代,诺和诺德(Novo Nordisk)和礼来(Eli Lilly and Company)合作在临床试验中评估一款M1/M4型毒蕈碱乙酰胆碱受体(mAChR)激动剂xanomeline治疗阿尔茨海默病(AD)的效果。当时,胆碱能假说是科学家们提出的AD病理机制之一,认为刺激胆碱能系统可能改善患者的认知功能。Xanomeline的设计构想是在患者的神经递质乙酰胆碱缺乏的情况下,通过直接激活M1/M4型毒蕈碱受体来刺激胆碱能系统,从而改善患者症状。
这款药物被推进到治疗AD的2期临床试验中,不过结果却不够理想,虽然它对患者的记忆能力有一定的改善,但是刺激外周毒蕈碱受体带来了一系列不良反应,包括恶心、呕吐和过度唾液分泌等。最终,xanomeline的研发进程被搁置。“因为我们觉得它在AD患者中没有表现出足够的安全性和耐受性。”当时负责这一研发项目的Steve Paul博士回忆道。
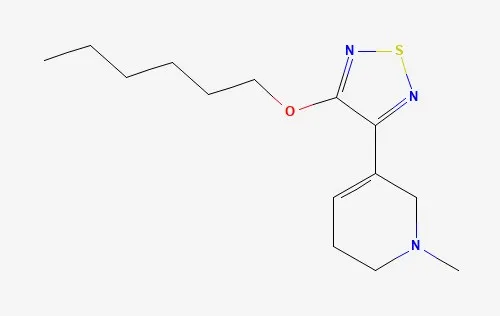
▲Xanomeline的化学结构(图片来源:PubChem)
不过,作为临床试验的一部分,研究人员发现xanomeline在治疗与AD相关的精神病发作(包括幻觉和妄想)方面表现出显著的效果。“这完全是意外的发现,”Paul博士表示,“我们没有想过它会发生。”研究人员在1997年发表了这一研究结果。
受到这项研究的启发,研究人员在一项小型临床试验中检验了xanomeline治疗精神分裂症患者的效果。在这些患者中xanomeline同样显示出疗效,不过不良反应仍然是阻止进一步研发的“拦路虎”。Xanomeline在精神分裂症方面的研发同样被搁置。而让这款药物“起死回生”的转机来自一位没有接受过正式神经科学和心理学培训的年轻人。
从被搁置到重获新生
2008年,Andrew Miller博士加入PureTech Health公司,他最初的任务是阅读文献和与研发人员交流,积累在新药研发方面的专长。在阅读和探索的过程中,他被精神分裂症导致长期严重残疾的特征深深触动。
Miller博士对精神分裂症的兴趣让他从文献中找到了被搁置的xanomeline,他和PureTech公司的同事意识到如果能够将xanomeline与不能穿过血脑屏障的毒蕈碱受体阻断剂联用,就可能在保留xanomeline在大脑中的抗精神病效力的同时,降低因为激活外周毒蕈碱受体带来的不良反应。

图片来源:123RF
他们通过文献查询发现了上百种毒蕈碱受体阻断剂,最终选择了trospium作为与xanomeline匹配的毒蕈碱受体阻断剂。这一组合成为了后来的KarXT。PureTech Health创建了Karuna Therapeutics公司,致力于推动KarXT的临床开发。而与这一分子颇有渊源的Steve Paul博士在从礼来公司退休后,也在2018年加入Karuna Therapeutics,成为该公司的首席执行官。
2019年,KarXT在2期临床试验(EMERGENT-1)中达到主要终点,不但显著改善了患者的精神分裂症阳性和阴性症状量表(PANSS)总分,还显示出良好的耐受性,患者因不良事件停药率与安慰剂组类似,未出现嗜睡或体重增加等其他常见抗精神病药物相关的不良反应。
2023年12月,百时美施贵宝(Bristol Myers Squibb)斥资140亿美元收购了Karuna公司。2024年,KarXT获得FDA批准(商品名Cobenfy),成为几十年来首个具有创新作用机制的抗精神病药物。
精神疾病药物研发的新方向
伴随着Cobenfy的成功,毒蕈碱乙酰胆碱受体靶向疗法的开发也成为神经系统疾病的重要研发方向之一。2024年在Nature Reviews Drug Discovery上发表的文章指出,这一领域有望迎来“黄金年代”,为阿尔茨海默病、精神分裂症等多种难于治疗的神经系统疾病带来具有全新机制的治疗选择。

百时美施贵宝正在多项3期临床试验中评估Cobenfy用于治疗阿尔茨海默病患者的精神病发作和激越症状的效果。与Cobenfy的作用机制类似,MapLight
Therapeutics开发的ML-007C-MA同样由M1/M4受体激动剂与外周作用的mAChR阻断剂组成,目前处于2期临床开发阶段,用于治疗精神分裂症及阿尔茨海默病相关精神病发作。
为了提高mAChR药物的亚型选择性,研究者转向别构调节剂。这些药物不与乙酰胆碱的活性结合位点结合,而是通过作用于mAChR的别构位点来调节受体活性。由于不同亚型的别构位点差异更大,这种方法有望带来选择性更强的新药。
在这一方向上,Neumora公司开发的NMRA-861是一款潜在“best-in-class”M4亚型mAChR正向别构调节剂(PAM),已经进入1期临床开发阶段。艾伯维(AbbVie)公司计划在临床试验中探索M4选择性PAM emraclidine作为附加疗法,与现有疗法联用治疗神经精神疾病的效果。
对mAChR结构更为详尽的解析,也推动了基于结构的药物设计。Nxera Pharma与Neurocrine Biosciences合作开发了一系列高选择性的mAChR激动剂。用于治疗精神分裂症的direclidine(M4亚型选择性激动剂)目前处于3期临床试验阶段。Neurocrine还有多款M1/M4激动剂在1期临床开发阶段。
改变精神疾病患者的生命
让我们回到文章开头的蒂姆,在接受Cobenfy治疗后,他开始主动与家人交谈,积极参加治疗小组,并提出想要尝试找一份兼职工作。更重要的是,他不再因不良反应而拒绝服药,终于能够稳定地坚持治疗了。他的医生,塔夫茨大学(Tufts University)神经科学系转化研究主任Michael Halassa博士表示,对于蒂姆来说,Cobenfy不只是另一款新药,而是一条生命线。
作为全球医药创新的赋能者,药明康德很高兴能助力合作伙伴,加速多款治疗精神疾病的创新疗法问世,造福病患。长期以来,药明康德都在支持全球合作伙伴从药物研究(R)、开发(D)到商业化生产(M)各个阶段的需求,通过独特的一体化、端到端CRDMO模式,助力更多药物加速从实验室来到患者身边。
以治疗精神疾病的小分子药物为例,药明康德化学服务平台能支持各种化学药物的分子形式及类别,满足从药物发现到商业化生产各个阶段、各个规模的各种物料需求。药明康德生物学业务平台作为综合性的早期发现和转化生物学赋能平台,能为包括精神疾病在内的多个疾病领域的新药研发提供从早期发现到临床研究阶段的生物学解决方案。药明康德测试业务平台可提供全生命周期的一体化研发测试服务及全方位的临床研究服务,助力合作伙伴的药物成功申报IND、NDA以及通过核查上市。
在这个世界精神卫生日,让我们向科学家、患者和所有推动创新的力量致敬。正是这些不懈努力,让越来越多的患者看到希望的曙光。药明康德将继续依托其“一体化、端到端”的CRDMO平台,加速合作伙伴的更多创新疗法问世,让科学的力量惠及每一位患者。
First in Decades! How a Once-Abandoned "Old Drug" Is Giving Patients New Hope
Schizophrenia is a common yet complex and serious mental illness that affects about 24 million people worldwide, according to the World Health Organization. Patients often suffer from hallucinations, delusions, disorganized thinking, and social withdrawal, symptoms that not only rob them of a normal life but also impose a heavy burden on families and society. Existing treatments can alleviate symptoms to some degree, but they remain limited by modest efficacy, treatment resistance, and significant side effects.
In recent years, breakthroughs in psychiatric drug development have reshaped the field, delivering the first novel mechanism therapy for schizophrenia in decades. This progress not only offers new hope for patients but also points to a broader shift in treatment approaches for mental illness. WuXi AppTec has long supported psychiatric drug discovery and development, leveraging its fully integrated, end-to-end CRDMO model to help partners efficiently transform scientific advances into innovative medicines. On this World Mental Health Day, we share the story of one patient to illustrate the possibilities that new therapies are bringing to this challenging area.
Lighting Up the "Light Bulb" in the Brain
Tim, a man in his twenties, was diagnosed with schizophrenia as a teenager. Over the years, he tried multiple antipsychotics, but the benefits were limited. Worse still, side effects such as weight gain, excessive drowsiness, and intolerable akathisia gradually eroded his willingness to stay on medication. As adherence declined, his symptoms spiraled out of control. His family described him as increasingly withdrawn, trapped in his own world, with a vacant gaze and bouts of agitation that he could not manage. His life became a cycle of hospitalizations and instability.
Everything changed in 2024 when Tim began treatment with Cobenfy (xanomeline/trospium). Within weeks, the "emptiness" in his eyes disappeared, replaced by vitality his family had not seen in years. Doctors referred to this as "the light bulb effect," as if a long-darkened bulb had suddenly switched on, revealing Tim’s personality and energy once more. For his family, it was the first real glimmer of hope. Yet the therapy that transformed Tim’s life had itself traveled a long and winding road to approval.
Originally Developed for Alzheimer’s Disease, with an Unexpected Effect
The story of Cobenfy begins in the 1990s, when Novo Nordisk and Eli Lilly and Company collaborated on clinical trials of xanomeline, an M1/M4 muscarinic acetylcholine receptor (mAChR) agonist, for Alzheimer’s disease (AD). At the time, the cholinergic hypothesis, suggesting that stimulating the cholinergic system could improve cognition, was widely studied. Xanomeline was designed to directly activate M1/M4 muscarinic receptors to compensate for acetylcholine deficiency, thereby improving symptoms.
Although xanomeline was advanced into Phase 2 trials, the results were mixed. While memory improved to some extent, activation of peripheral muscarinic receptors triggered adverse effects such as nausea, vomiting, and excessive salivation. Ultimately, the program was shelved. "We felt it didn’t show sufficient safety and tolerability in AD patients," recalled Dr. Steve Paul, who led the project at the time.
Yet amid these disappointing results, researchers noticed something surprising: xanomeline had a significant effect on AD-related psychosis, including hallucinations and delusions. "It was completely unexpected," Dr. Paul noted. "We didn’t think it would happen." The findings, published in 1997, sparked further curiosity.
Encouraged, xanomeline was tested in a small group of schizophrenia patients. The drug again showed signs of efficacy, but intolerable side effects halted further development. Once more, xanomeline was shelved, until an unlikely champion emerged: a young scientist without formal training in neuroscience or psychology.
From Shelved to Reborn
In 2008, Dr. Andrew Miller joined PureTech Health, initially tasked with reviewing literature and engaging with researchers to build expertise in drug development. While doing so, he was struck by the profound disability caused by schizophrenia.
Digging deeper, Dr. Miller rediscovered xanomeline. He and colleagues at PureTech recognized that pairing xanomeline with a peripherally acting muscarinic antagonist, one unable to cross the blood-brain barrier, might retain its antipsychotic activity in the brain while reducing peripheral side effects.
After screening hundreds of candidates, they identified trospium as the best match. This combination became KarXT. To advance it, PureTech Health founded Karuna Therapeutics. In 2018, Dr. Steve Paul, who had once led the xanomeline development, joined Karuna as CEO, bringing the story full circle.
In 2019, KarXT met its primary endpoint in the Phase 2 EMERGENT-1 trial, significantly improving the Positive and Negative Syndrome Scale (PANSS) scores. Importantly, tolerability was favorable: discontinuation rates due to adverse events were similar to placebo, and the common side effects of traditional antipsychotics, such as somnolence and weight gain, were not observed.
Momentum built quickly. In December 2023, Bristol Myers Squibb acquired Karuna for $14 billion. By 2024, KarXT was approved by the FDA under the brand name Cobenfy, marking the first antipsychotic with a novel mechanism in decades.
A New Direction for Psychiatric Drug Development
Cobenfy’s approval signaled more than the success of one drug; it reignited interest in muscarinic receptor-based therapies. A 2024 article in Nature Reviews Drug Discovery described this area as potentially entering a "golden era," with novel mechanisms offering new options for Alzheimer’s disease, schizophrenia, and other hard-to-treat conditions.
Bristol Myers Squibb is now conducting multiple Phase 3 trials to assess Cobenfy in AD-related psychosis and agitation. Similarly, MapLight Therapeutics is developing ML-007C-MA, a combination of an M1/M4 agonist with a peripherally acting muscarinic receptor antagonist, now in Phase 2 for schizophrenia and AD-related psychosis.
To further refine the approach, researchers are focusing on subtype selectivity. Allosteric modulators, agents that bind to receptor sites distinct from acetylcholine’s binding site, are emerging as a promising solution, as differences among allosteric sites can allow for greater subtype specificity.
Neumora’s NMRA-861, a potentially "best-in-class" M4 positive allosteric modulator (PAM), is already in Phase 1. AbbVie, meanwhile, plans to explore the M4-selective PAM emraclidine as an add-on therapy in neuropsychiatric disease trials.
Advances in mAChR structural biology are also fueling structure-based drug design. Nxera Pharma and Neurocrine Biosciences are co-developing a portfolio of highly selective agonists, including direclidine (an M4-selective agonist) now in Phase 3 for schizophrenia. Neurocrine also has multiple M1/M4 agonists in Phase 1 development.
Changing Patients’ Lives
Returning to Tim’s story, the impact of Cobenfy has been profound. He began conversing with his family again, actively joined therapy groups, and even expressed interest in part-time work. Most importantly, he no longer refused medication due to side effects and could finally remain on consistent treatment. For Tim, said Dr. Michael Halassa, director of Translational Research in the Department of Neuroscience at Tufts University, Cobenfy was not just another drug, but a lifeline.
As a trusted partner to innovators worldwide, WuXi AppTec plays a vital role in advancing the next generation of therapies for neurological and psychiatric diseases, including schizophrenia, through its integrated CRDMO platform. By combining scientific expertise with integrated global infrastructure, WuXi AppTec enables faster, more efficient progress across the entire drug development lifecycle.
For small-molecule innovation, WuXi AppTec’s Chemistry Services Platform supports all categories of chemical compounds and production scales. This infrastructure helps partners meet material needs from lead optimization to clinical supply and beyond. Meanwhile, WuXi AppTec’s Biology Business Unit offers an integrated platform for early discovery and translational biology, empowering researchers to evaluate new targets and mechanisms in neurological diseases with precision and speed.
WuXi AppTec’s Testing Division enhances these capabilities with comprehensive R&D testing and clinical research services. From preclinical safety assessments to IND/NDA-enabling studies, the team helps streamline regulatory submissions and approval processes. This integrated model not only accelerates timelines but also enhances efficiency—helping transform innovative ideas into life-saving therapies.
Looking Forward
On this World Mental Health Day, we honor the scientists, patients, and all those driving innovation forward. Through their tireless efforts, more and more patients are seeing a brighter future. WuXi AppTec will continue to leverage its fully integrated, end-to-end CRDMO platform to help partners bring more groundbreaking therapies to life, ensuring that the power of science reaches every patient.

 产业资讯
产业资讯
 生物制品圈
生物制品圈  2025-12-08
2025-12-08
 77
77

 产业资讯
产业资讯
 医药魔方Pro
医药魔方Pro  2025-12-08
2025-12-08
 60
60

 产业资讯
产业资讯
 医健大观
医健大观  2025-12-08
2025-12-08
 61
61